Let's Connect
Our friendly and educated team is here to partner with you every step of the way. Connect today to learn of all the ways to partner with The Common Market.
Food as Medicine programs are gaining a lot of traction as potential solutions for addressing key social determinants of health within healthcare systems, specifically for higher risk patients in underserved areas. The Common Market has teamed up with a number of healthcare systems to support these initiatives by providing our Farm-Fresh Boxes, a curated box of fresh, seasonal produce to healthcare systems including Sanitas Medical Center, Children’s Hospital of Pennsylvania, and Lankenau Medical Center, among others.
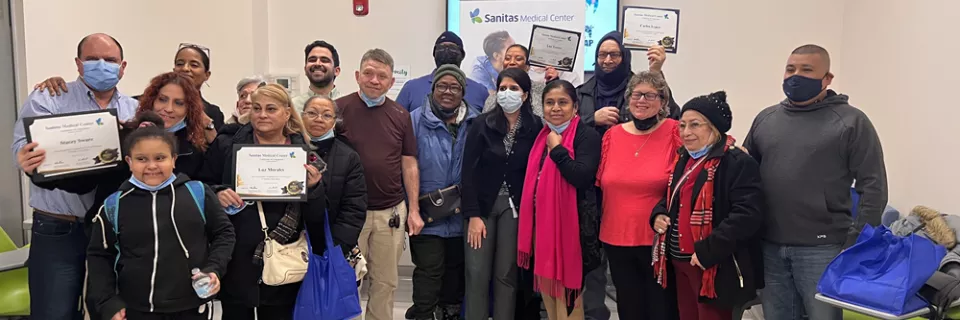
Sanitas Medical Center’s program includes a home delivery of fresh fruits and vegetables to program participants on a weekly basis. Beyond addressing food insecurity, the program has clear clinical objectives, including reducing A1C, addressing HEDIS Preventative Measures, and closing “Care Gaps” related to these measures.
Sanitas formed innovative partnerships in order to bring its program to life, including ones with The Common Market and Food Connect Group, an organization that has helped execute at-home deliveries for patients using last-mile delivery and SMS text-based communication solutions.
To get the full scoop on the impact of these programs on the communities they serve, and potential barriers to scaling these programs, Katie Barr from our team sat down with one of our partners, Dr. Rashi Sharma of Sanitas Medical Center to chat about the success of their three-year-old Food as Medicine program.

Katie Barr: To get us started, can you briefly describe for us what a Food as Medicine program means to you, the different kinds you've encountered, and how you've implemented your own program at Sanitas Medical Center?
Dr. Rashi Sharma: Food as Medicine, to me and to my organization, is basically helping patients understand what food is, and how it plays an important role in impacting their health. One could say that it sometimes plays a bigger role than their medicines. It's basically helping our patients, and thereby helping our communities, understand what role food has in terms of their health.
I haven't really encountered many other Food as Medicine programs; I only started learning about them when we started our own program here, two or three years ago. I know the Rockefeller Foundation and various universities have programs where they're teaching health care providers, community advocates, and patients about Food as Medicine.
I think healthcare providers play a vital role in making that connection to patients. So, I'm definitely starting to learn more about the different programs, how they work, what settings they're in, etc.
We serve a primarily underserved community that has more social determinants of health than just food access, but food access is a big one. I think that's an important thing to consider for anybody. Where you're working, is there a food access problem? And can that help you get started in implementing the program?
We started our own program at Sanitas in 2021. We decided to have this food program for our patients in just one of our three locations here in New Jersey, but we pre-selected for patients that had diabetes or prediabetes because we found that they were at higher risk for healthcare complications based on what they were eating, and what they understood about food. We also pre-selected based on the patients that our healthcare providers thought were likely to attend, and were physically able to attend the sessions.
We started the program from the ground up. Our CEO reached out to local food banks to try to create a relationship, then we established last mile delivery since all of our patients were in one county at that point. We then expanded to our Union City office; that's where The Common Market became a vital partner. Our partners at Food Connect Group helped get food to more patients in different geographic areas. So, we started it from the ground up, found these partners, pre-selected the patients ourselves, and then held monthly sessions with the patients, one session in English, one in Spanish.
Initially, it was a six-month program. The very first year, the plan was to have MEND (Meeting Essential Needs with Dignity), which was the food bank partner in Belleville at the time, provide fresh produce weekly for three months. But given the engagement and the success of the program, even in those first three months, they decided to extend it for six months. And so that's what we've been doing since then. And it's been great!
KB: You mentioned a lot of variables for pre-selecting certain patients within a specific radius, and working with different partners. What were some of the most important aspects of developing this program?
RS: Right, the most important things are interest and engagement; understanding that this is a need for our patients, that this is a roadblock to them achieving their healthcare goals.
Our organization as a whole likes to enable patients to be more in charge of their healthcare goals. So, it's not me saying, “Hey, your A1C is 10, you have to get it down to this.” It's: “Do you understand what an A1C means? What do you want out of this? This is the potential list of complications that are going to happen, and how do I help you? What do you want?”
We ask them: “What are your goals?” – that's how we get our patients more engaged because it's not their doctor telling them what to do. It's them saying, "This is what I want, I want to be healthier, I want to be able to wake up in the morning without this issue. I want to be around for the next five years without these issues, because of A, B, and C." It's incorporating what drives them into their healthcare plan, so to speak, it's like a self management plan. So having this program succeed is very largely dependent on the buy-in from the patients, for sure.
And definitely, our team's buy-in as well – healthcare providers, our doctors, nurse practitioners, and care coordinators who work directly with the patients in the program. Our operations team helps us navigate logistics, the care coordinators and the Registered Dietitian lead the sessions, and the providers are there to help answer patients' questions on clinical topics, which inevitably come up when we're talking about food.
It's engagement from all sides: patient engagement, team engagement, getting the community engaged. That's the only way that we've made this work.
KB: Fantastic. Yeah it sounds like it really depends on the people in those environments when you are putting those programs together. You mentioned interest, engagement, and buy-in from the patients are the most important things. But, I'm curious, what are some of the strategies that you might employ to ensure participation and interest among patients?
RS: Yeah, that's definitely one of the hurdles we've encountered over the last three years of doing this program. The primary care providers talk to their patients about it months before the program starts, and tell them why it's so great. A lot of people are very interested when we start, but then there are inevitable issues of not being able to make it on time or missing several sessions.
Our program only includes six sessions; if the participant misses more than two sessions, they are technically out of the program. Missing two sessions makes it difficult for us to measure impact and analyze results.
The two session absence limit does make it hard for some patients. But, we try to make it easier by holding the sessions in two different centers. So twice a month, our whole team goes to one center one week, and then another center the following week. I've seen over the last two years that patients will go to the other center when they've missed a session. Our care coordinators are also extremely engaged; they'll call them and remind them the week before the session, or the day before the session.
One of the motivations behind pre-selecting patients is to ensure that we have active and committed patient engagement. They do intake with our care coordinators before the program starts, which gives them details on the food delivery, the sessions, and the parameters that we're trying to measure as well.
We know that we live in a very virtual world, but right now our sessions are in-person. We haven't quite worked out a virtual option if they can't make it in-person. But we're trying to figure out how to incorporate that in the best way. And I know we can definitely reach more patients that way, too.
KB: I can appreciate that a virtual component is challenging to implement when you have so many different moving parts, and different languages as well. Given the success of your program, how do you feel the program has helped participants maintain those numbers and lifestyle changes, if it has? And if not, what are some barriers to maintaining some of those behaviors?
RS: Yeah, we've been following our cohort of patients that were in the program last year, for example, over the course of the past six months. They were in the program from June 2022 to December, and then we followed them over the following six months, and we saw that a lot of them were able to stick to their goals; their A1Cs were stable.
With one of my patients, her sugar levels gradually started increasing again as soon as the program ended.
And, so I asked her: "What's going on? Is it the medications, is it what you're eating, did your physical activity change?"
And for her, specifically, the issue was her food. She said she just was not eating the same way. She said she loved the program, but with patients like this they say it's either a time issue, an understanding issue, or a consistency issue.
Our strategy here is engagement and consistency. Our team stays in touch with them. Our patients with diabetes are part of our subset of high-risk patients that we follow more closely via our care coordinators, so they're getting the outreach phone calls and messages telling them they need to see their provider for follow-ups and exams. And by doing that, we're also engaging them in other preventative health measures, such as mammograms. The main thing is making sure the team has the resources to stay consistent with that outreach.
KB: It sounds like you all are doing a fabulous job of making sure that you stay in touch with your patients and still ensure that those resources are available. As a quick follow up, do you have additional resources that you provide patients after the program ends?
RS: Yes. At the start of each program, during the first session we go through some resources on SNAP, local food assistance, financial assistance, and how to contact their community advocates.
We give patients a folder, kind of like a syllabus, that has all the resources listed in English and in Spanish. It also contains contact information for our care coordination team, so they feel encouraged to contact them directly and ask for support and assistance. We obviously can’t solve every issue; we have a small team right now, but a very committed team. So we're always looking for ways that we can help when we can't provide the answer.
KB: Absolutely. I'm going to shift gears a bit and ask about the food side of the program. How did local sourcing play a role in your program?
RS: Local sourcing for us was very important because one of our core values is community and community building. Local sourcing falls into that. We want our patients to know that there are people like them that are doing the same work, that are trying to support them. For me, local sourcing adds a personal touch. It's more relatable, sometimes more accessible, and affordable than saying: "Go to whatever big chain store and get your vegetables," which are probably marked up, especially if they're organic. And for our patients, that's not part of their routine, it's not part of their culture to do that either. So local sourcing helps us stay a little bit more connected to the community and engage our patients in their own communities.
Our goal, our primary commitment, is to support our patients. We know that whoever the local farmers are, the local food producers, they may not be our patients on paper, but they're part of the community that we're serving. And so on a values level, where we place our effort and our money is important to us. Where we do business is also important for our region.
KB: In what ways do you feel these programs can potentially scale up and be brought to other healthcare systems, if they can?
RS: Oh, they can definitely be scaled up. What we do right now is very small scale, but the impact is huge. It's so wonderful to see our patients benefit from this and have a team where everybody knows each other. We're bouncing ideas off each other all the time. But, we have a very small footprint right now in New Jersey. I think these programs can definitely be scaled up, especially in organizations or places where they have more hands, more people, more resources to work with.
I think it's great that we have these two sessions twice a month. But, I think the best thing would be making it more flexible for our patients: having classes throughout the week and on the weekends, having more virtual sessions, having coaches or coordinators that are present on demand for patients when they have questions or needs, having resources ready at your fingertips to give to patients about what is available in your community, how they can access food and what to do with it when they get it.
I think there are ways to scale it up for bigger healthcare systems…when you have the resources to appeal to a much larger population, and have the flexibility with time.
KB: That's so inspiring to hear that there is the potential and possibility for this to be able to branch out. Is your team working in any capacity to try to scale this work, or to provide additional inspiration or resources for other healthcare systems to replicate it?
RS: Our team is very involved with our local communities where our practices are, and we have community health workers, community ambassadors that are very present in the community. Our hope is to have them more involved in our sessions in the future, creating a bit more of a presence in front of our patients, so that they see that everyone's involved. It's patients connecting to other patients, it's patients connecting with us, it's patients connecting with the community, and it's us connecting with the community and building those bridges. We are looking to do that on a bigger scale, and we definitely need more people and funding to do that. But, we're looking into that with the amount of resources that we have now. It's definitely one of our goals.
KB: What are some of the major barriers to scaling this up or implementing it in other locations?
RS: Funding is a big one, right? We are a for-profit organization at Sanitas. So, we have some limitations on what we can do. Working with nonprofit partners like The Common Market and Food Connect is critical as it pertains to sourcing food and getting it to our patients.
Other social determinants of health definitely play into consistency, which is the biggest barrier. Can patients attend the sessions? Do they have the financial resources to go out and get food like this on their own? Do they have housing stability? A lot of patients that we serve do have to choose between rent and food. Sometimes it's easier to get fast food because it's cheaper. There's a lot of inequity that we come across when it comes to food, when it comes to housing, financial inequity, and racial disparities. All of those definitely play into the barriers that we try to overcome; there's only so much we can do about all of those, but sometimes lending an ear and giving some support to our patients helps. But, there are inevitably a lot of barriers.
KB: Yeah, I can appreciate that. Sometimes it might feel like pushing a boulder uphill or like taking two steps forward, three steps back when you come up against some very serious systemic inequalities. Given all of the barriers and wonderful elements you have described of these programs, what is some advice that you would have for other medical professionals or healthcare systems if they do want to start their own Food as Medicine program?
RS: I would say start, don't wait. Don't wait till you have everything in order. If you have a few hands on deck, and you're able to make relationships with partners, such as The Common Market, just start. It's not going to be perfect. We've been doing this for three years now, and it's definitely not perfect. But we saw the impact, even in the first year, on our patients. I would say just start, the need is there. If you just open your eyes, look around, you see that there's food inequality everywhere. And if you have an idea, share it with your team! Someone else might have resources or ideas that they can bring in to link it into a bigger project. So I would just say, don't wait. Just start with whatever it is.
KB: You adjust and adapt alongside it. That's fantastic. We truly value and appreciate the work that you do. Do you have anything else that you'd like to add?
RS: This is such a fun program for me to do. We've been doing this for three years now. Union City is where I've been seeing patients for the last five years. Last year for me was very, very special, because I would attend the sessions, and my own patients were a part of the group. Seeing them so engaged, seeing them improve over the course of the six months without any adjustments in their medication, and just adjusting their food was so wonderful. They were all so happy and seeing them interact with my team also made me very happy. Seeing them interact with each other too, it's such a special thing. Can we scale that feeling up?
KB: Yes! That feeling of giving back to and being a part of your community is so invaluable, there's no price you could put on that. And I am so excited that you've had this opportunity to be able to build this out for your community as well.
RS: Thank you so much. You know, The Common Market has definitely been such an integral component of that. We couldn't have achieved what we've done without your support. So thank you, too.
Want more?
Catch Dr. Rashi Sharma in the webinar Farm-to-Door: Meeting Patient Needs via Technology & Good Food as part of the 2023 Nutrition Incentive Hub’s National Convening at this link.
An Executive summary of the results of a Food as Medicine (FaM) program can be found here.
Additional resource
For more information on Food as Medicine programs, check out the Milken Institute's report on Market Solutions for Scaling Food Is Medicine Prescriptions.
Our friendly and educated team is here to partner with you every step of the way. Connect today to learn of all the ways to partner with The Common Market.
"The Common Market has been wonderful to work with. Not only is the customer service great but the products are also."
— Derick Smith, Culinary / Culinary Purchaser, Cancer Treatment Centers of America